Perimenopause vs. Menopause vs. Post‑Menopause: What’s the Difference?
Women’s midlife hormonal transitions are complex, but understanding them empowers better health and wellness decisions. Although many people use “menopause” as a catch‑all term, perimenopause, menopause, and post‑menopause are distinct phases with specific biological definitions, symptoms, and health implications. Read on to discover exactly how they differ — with insights from scientific research and expert clinical sources.
What Is Perimenopause? The Transitional Phase
Perimenopause (literally “around menopause”) is the biological transition period preceding the end of menstrual cycles. It can span 2 to 8 years and is marked by erratic hormonal activity and symptoms that often resemble those of menopause itself.
Key features
Estrogen and progesterone levels fluctuate wildly as ovarian function declines.
Menstrual cycles become irregular — shorter or longer, heavier or lighter.
You may still ovulate occasionally, so pregnancy is possible until full menopause.
Common symptoms
Perimenopause often includes:
Hot flashes and night sweats
Mood swings, anxiety, depression
Sleep disruption and fatigue
Brain fog and concentration issues
Changes in sexual desire
These symptoms reflect both hormonal shifts and their impact on neurological systems.
Science insight: Research characterizes perimenopause as a unique metabolic and hormonal transition with implications for cardiovascular and metabolic health well before menopause begins.
Menopause: The Biological Milestone
Menopause itself is not a long period — it’s a point in time. Clinically, menopause is defined as 12 consecutive months without menstrual bleeding.
How it works
Your ovaries stop releasing eggs, and estrogen and progesterone drop to low levels.
This cessation of reproductive hormone production signals the end of fertility.
Typical age
Most people reach menopause around age 51, though this can vary.
Symptoms
Many symptoms that start in perimenopause continue into menopause and beyond, including:
Hot flashes
Vaginal dryness
Sleep problems
Mood changes
These occur due to sustained low estrogen and ongoing physiological adaptation.
Important distinction: While perimenopause may last several years, menopause is a definitive diagnostic milestone based on the absence of menstruation for one year.
Post‑Menopause: The Long‑Term Phase
Post‑menopause begins the day after you’ve gone a full year without a period. It continues for the rest of life.
What happens biologically
Estrogen levels remain low — and this sustained deficiency affects multiple systems.
While some symptoms fade, others may persist or emerge due to long‑term hormone deficiency.
Common post‑menopausal health considerations
Increased risk of osteoporosis due to decreased bone density
Greater susceptibility to cardiovascular disease
Potential metabolic changes
These are linked to long‑term low estrogen states and are why health monitoring remains important after menopause.
Why These Distinctions Matter — Beyond Labels
Understanding the differences between these stages isn’t academic — it affects:
Clinical care and symptom management
Timing and type of hormone therapy support
Monitoring for bone, heart, and metabolic health risks
For example, hormone therapy may offer benefits when initiated near menopause but different risks if started later in post‑menopause.
And because symptoms like vasomotor issues and mood changes can vary by stage, targeted strategies may help each phase more effectively.
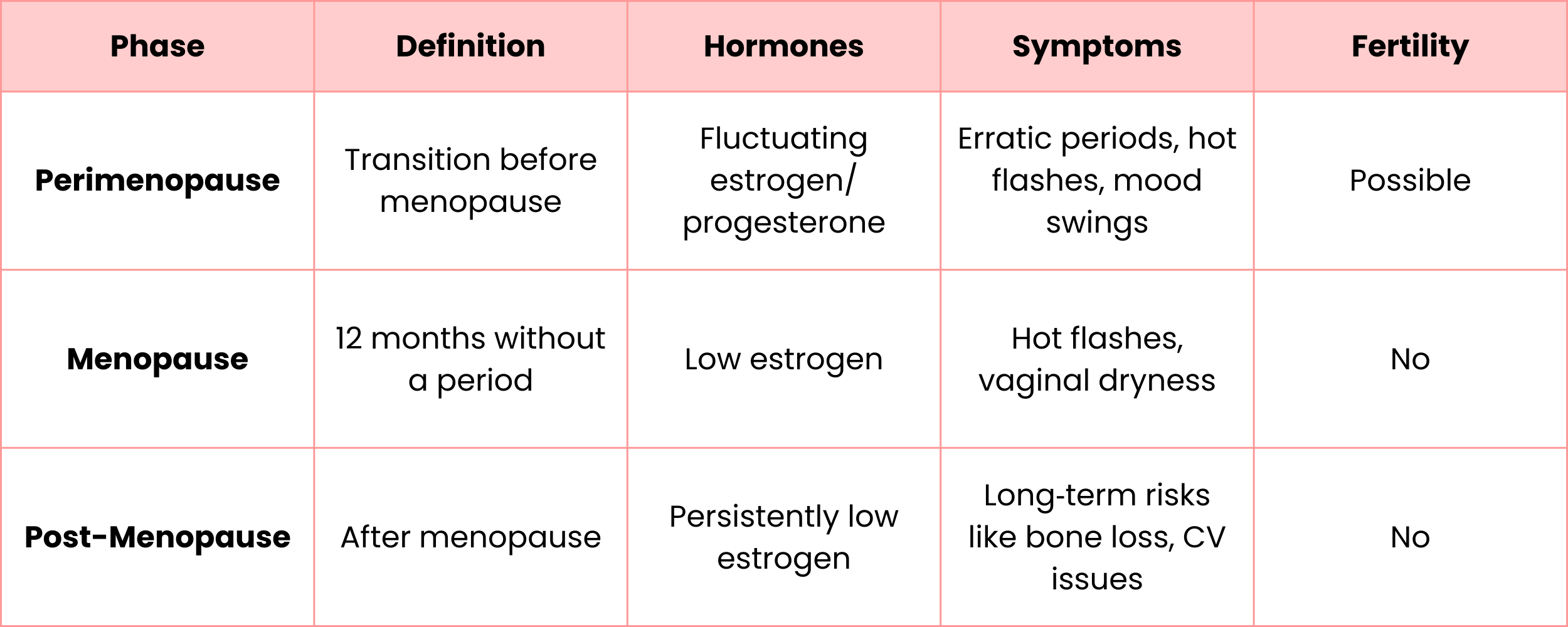
A Quick Summary
Final Thoughts
The journey through perimenopause, menopause, and post‑menopause is neither linear nor uniform — but knowing what each stage is helps women make decisions about lifestyle, medical care, and overall wellbeing. With consistent follow‑up and supportive health strategies, midlife transitions can become a period of empowerment rather than confusion.
Editor’s note: At Hello Mamas, we love sharing great health and wellness tips, but this is not medical advice. Always consult your doctor or healthcare team before starting any new routine or treatment. Also, at Hello Mamas, we share products we personally love and may earn a small commission from affiliate links. This doesn’t affect the price you pay. We only recommend products we genuinely believe in, but your experience may vary.